

You can’t keep Kaleb Stewart down now that surgery addressed the back pain the 18-year-old had been living with for a few years.
Kaleb’s mom, Patty, said he first complained of back pain around age 13. She initially thought it was growing pains – he was going through a growth spurt and was also an avid dirt bike rider. Kaleb said the pain would vary from sharp to numbness and tingling that would travel all the way to his feet.

Rockford Spine Center’s Dr. Michael Roh and his team recently attended the Cervical Spine Research Society’s 47th Annual Meeting in New York City, where topic highlights included cervical disc replacements and management of asymptomatic spinal cord compression.
Mark McDonnell could hardly walk or drive because of intense pain along his right side for several months in 2018.
Rockford Spine Center physicians Michael Roh, M.D., Christopher Sliva, M.D., Fred Sweet, M.D., and Marie Walker, M.D., were recently recognized by Vitals with the On-Time Doctor Award for 2019. This is the sixth consecutive year the physicians have received this award.
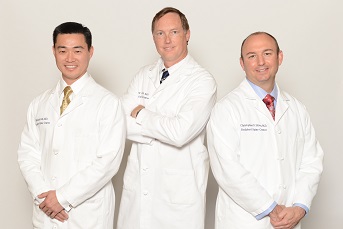
Rockford Spine Center physicians Michael Roh, M.D., Christopher Sliva, M.D. and Fred Sweet, M.D. were recently named to the America’s Most Honored Professionals 2019 list.

A routine pediatrician visit back in 2015 led Taylor Brown to not only learn about scoliosis but also educate others about the condition through her love of dance.

Rockford Spine Center’s Dr. Michael Roh recently attended an international scoliosis conference where world experts gathered to discuss the treatment of scoliosis and complex spinal deformity.

When he is not working in Springfield, Illinois Senator Dave Syverson enjoys playing regular games of basketball and baseball, but a recent back injury sidelined him from his normal active routine.
Rockford Spine Center physicians Michael Roh, M.D., Christopher Sliva, M.D., and Fred Sweet, M.D. were recently recognized with the Castle Connolly Top Doctors award. The doctors have been named to the list for seven years in a row. Only 4%-5% of doctors in America earn this prestigious honor.
Rockford Spine Center will continue to serve as a member of the Rockford IceHogs Medical Network for the 2019-2020 season. Michael Roh, M.D., Christopher Sliva, M.D., Fred Sweet, M.D., and Marie Walker, M.D. are members of the secondary medical network as the team’s orthopedic spine specialists.
It’s been more than a decade since Caroline Kelly Wright was regularly swapping walking for crawling because intense back pain interfered with her ability to stand.
Rockford Spine Center physicians Michael Roh, M.D., Christopher Sliva, M.D., and Fred Sweet, M.D. were recently recognized by Vitals with the Compassionate Doctor Recognition for 2019. This is the ninth consecutive year the physicians have received this award.
Beth Goetsch thought of Dr. Fred Sweet immediately when her lower back issues and nerve pain returned nearly 20 years after they’d first met.

Rockford Spine Center physicians Michael Roh, M.D., Christopher Sliva, M.D., Fred Sweet, M.D., and Marie Walker, M.D., were recently recognized by Vitals with the prestigious Patient’s Choice Award for 2019. This is the ninth consecutive year all four physicians have received this award.
When 63-year-old Roscoe resident Susan Russell experienced back pain so intense that she could no longer get on and off her motorcycle, she knew it was time to seek professional medical treatment.

Dana Horak trusted her instincts about her daughter’s back issue, which started the journey of navigating scoliosis diagnosis and treatment.

Jake Bradt can easily recall when his back pain became a problem and would go on to affect the next two years of his life.

Rockford Spine Center’s Dr. Christopher Sliva recently traveled to Seattle for training on a minimally invasive surgical technique to help people suffering from lower back issues.

Rockford Spine Center’s Dr. Michael Roh recently spoke with physicians at the University of Southern California’s Keck School of Medicine about his work with a medication that helps patients better manage post-operative pain.

A back injury derailed Cynthia Jemmott’s quality of life in Barbados with no hope of improvement for several years.

Zeb Lappin easily recalls the day his back went out – Oct. 13, 2013. He was working out doing squats when something happened that caused excruciating pain.

Jeff Kaney’s business is aerospace but he never expected an airplane ride to be crucial to his recovery from a back injury.

Kevin Finnegan loves to exercise. For many years, he enjoyed weight-training along with a full range of sporting activities. His back periodically would bother him, which he attributed to poor form while lifting weights. But five years ago, in the middle of a tennis game, he found himself having intense pain in the back, buttock and leg.

Rockford Spine Center’s Dr. Fred Sweet was the senior author on an important study about antibiotic use during surgery, a writeup of which recently appeared in The Journal of Bone and Joint Surgery.

Rockford Spine Center will continue to serve as a member of the Rockford IceHogs Medical Network for the 2018-2019 season. Dr. Michael Roh, Dr. Christopher Sliva and Dr. Fred Sweet are members of the secondary medical network as the team’s orthopedic spine specialists.